Back to all News & Events >
Author Archives: WHRI

CIHR Project Grants Spring 2024 Results
Congratulations to the recipients for the Canadian Institute of Health Research 2024 Spring Project grants! We are especially proud of our WHRI members (bolded) receiving these awards. Project Grants aRtificial intelligence-driven computational pathology platform for blAdder Cancer subTyping (REACT) Link to Abstract: Here Principal Investigator: Bashashati Ali Black, Peter C Wang, Gang Institution Paid:University of […]

Introducing the Bone Metastases Exercise Hub!
It is now well established that exercise is highly beneficial in managing the side effects and symptoms of cancer diagnosis and treatment. However, historically, people living with advanced cancer (incurable or metastatic disease) have not been included in research studies, and rehabilitation and exercise prescriptions have been underutilized despite the potential to improve physical function […]
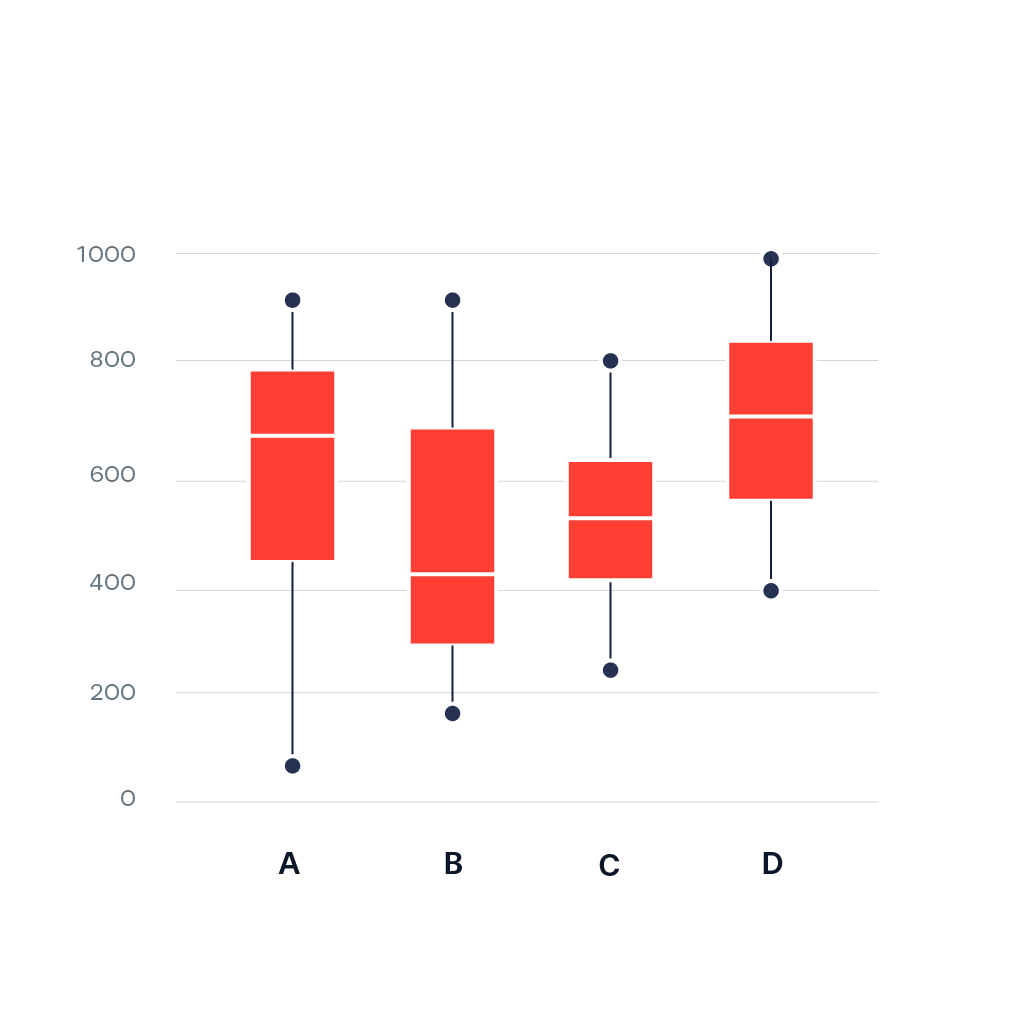
Sabina’s Stats Corner: Understanding Box Plots: A Comprehensive Guide
Special Notes: Listen to our L&L lectures online: WHRI Lunch & Learn Series – Women’s Health Research Institute Visit our Stats corner in the e-blast for previously published tips on data management and analysis: E-Blast Archive – Women’s Health Research Institute (whri.org) We are back! Today, we dive deep into one of the most fundamental yet powerful […]

Announcing the Trainee Travel Grant Spring 2024 Recipients
The WHRI congratulates the recipients of the 2024 Spring Trainee Travel Grant. As part of the WHRI’s Strategic Plan 2019–2024, the Trainee Travel Grant supports full-time research trainees for travel to national or international meetings. Ten grants valued at up to $1000 each are offered annually, with 5 grants available in May and 5 in […]

Celebrate World Sexual Health Day 2024 with the WHRI!
World Sexual Health Day (WSHD) is an annual awareness day managed by the World Association for Sexual Health (WAS). As a global advocacy organization, WAS is dedicated to promoting best practices in sexual health. Taking place on September 4th, WSHD aims to dismantle social and cultural taboos surrounding sexuality while advocating for positive sexual health […]

Updates to the Perinatal Data Registry
We are excited to announce a new data linkage available with the BC Perinatal Data Registry (BCPDR). As of June, we can now link BCPDR data to neighborhood-level socioeconomic status (SES) data and deprivation indexes. Previously, researchers could not access SES information without a lengthy application process. Through the WHRI, researchers can now access publicly […]

Pride 2024 and Going Beyond the Binary
WHRI acknowledges the history of Pride as a movement toward justice, and how health-care systems can perpetuate inequities in 2SLGBTQIA+ wellbeing. In alignment with the month of June signifying Pride Month (as well as the start of the longer Pride season), we celebrate and honour the contributions of 2SLBTQIA+ peoples in forging a fairer and […]

Sabina’s Stats Corner: Improving Statistical Inference of a Self-Selected Sample
Special Notes: Listen to our L&L lectures online: WHRI Lunch & Learn Series – Women’s Health Research Institute Visit our Stats corner in the e-blast for previously published tips on data management and analysis: E-Blast Archive – Women’s Health Research Institute (whri.org) You don’t have to be an expert to create a survey, but by following a […]

Mental Health Awareness Month
May is Mental Health Awareness Month May is Mental Health Awareness Month. This month is dedicated to educating, informing, and raising awareness about mental health. In honour of Mental Health Awareness Month, we’ve curated a collection of mental health resources connected to women’s health care research. This month is an opportunity to shine light on […]